Table of Contents
- What is Gingivitis?
- What Are the Gingivitis Symptoms?
- How Does Early Stage Gingivitis Look?
- What Causes Gum Disease and Gingivitis?
- How Does Plaque Cause Gingivitis?
- Do Gingivitis Cuts on Gums Indicate Severity?
- How to Treat Gingivitis?
- Prevention of Gingivitis
- Complications If Gingivitis Is Left Untreated
- Final Takeaways: Take Gingivitis Seriously
- FAQs
Oral health is vastly neglected, yet it is important for overall well-being. Among all the common dental problems, the most important one is gingivitis, which is the earliest stage of gum disease. It may begin with mild irritation, redness, or a slight tendency of the gums to bleed. Untreated gingivitis can progress into periodontitis, a severe condition that can lead to tooth loss and affect systemic health.
While it may begin silently with mild irritation, redness, or bleeding of the gums,
According to the CDC , approximately 47% of adults 30 and older exhibit signs of gum disease, and gingivitis is the precursor for most. The great news? Gingivitis is both preventable and reversible when caught early.
This blog explores what gingivitis is, its symptoms, early warning signs, causes, and treatment options, giving you the knowledge to take control of your gum health.
What is Gingivitis?

Gingivitis is one of the most widespread types of gum disease, but many people don’t realise they have it until it worsens. At its simplest, gingivitis is the inflammation of the gums, most often caused by plaque buildup on the teeth. Plaque is a sticky, invisible film of bacteria that constantly develops on your teeth. If it isn’t removed, it can harden into tartar, irritate your gums, and lead to bleeding or swelling.
Unlike more severe gum diseases such as periodontitis, gingivitis can be reversed when treated early. But if left untreated, it can harm the tissues and bones that hold your teeth in place.
Key facts:
- Gingivitis is the earliest stage of gum disease.
- It appears with mild signs such as redness, swelling, or bleeding gums.
- With the right care, gingivitis can be reversed before it becomes a serious problem.
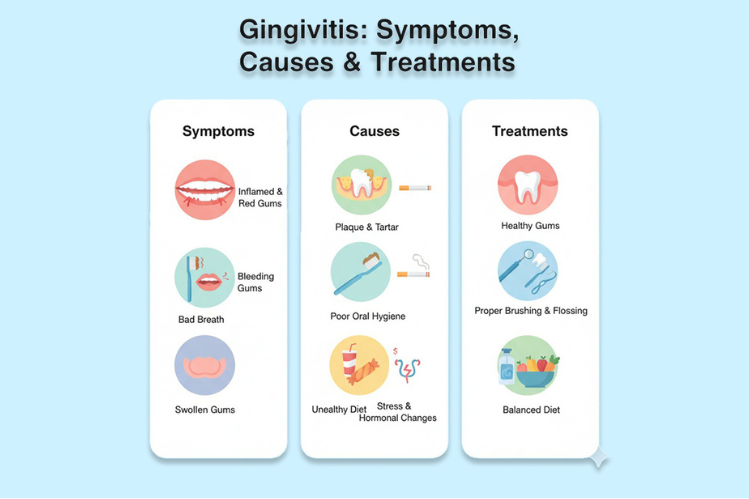
What Are the Gingivitis Symptoms?
- Red, Swollen Gums: Healthy gums should normally look pink and feel firm.
- Bleeding Gums While Brushing or Flossing: This is often one of the first warning signs.
- Persistent Bad Breath (halitosis): Caused by bacteria feeding on plaque buildup.
- Gum Tenderness or Pain: Discomfort when brushing, flossing, or eating.
- Receding Gums: Gums begin to pull back, making teeth look longer.
- Small Gum Cuts or Sores: Inflammation can make gums more fragile and prone to tiny injuries.
How Does Early Stage Gingivitis Look?
In its early stage, gingivitis usually shows up as:
- Mild gum swelling or irritation
- Light bleeding during brushing
- Slight sensitivity in the gums
At this point, the condition is still reversible.
What Causes Gum Disease and Gingivitis?
Here are the causes of gingivitis:
Poor Dental Hygiene
Dentists recommend brushing twice a day with antibacterial toothpaste, flossing daily, and using an antibacterial mouthwash to stop plaque buildup. Plaque is a sticky, yellowish film of bacteria that forms when teeth aren’t cleaned properly. The acids from plaque attack enamel and irritate gums, making poor dental care the top cause of gingivitis.
Age
As you get older, natural changes like reduced saliva production happen. This makes older adults more likely to develop gingivitis and periodontal disease.
Genetics
Family history matters too. If your parents had gingivitis, your risk increases since certain bacteria are often passed on early in life.
Crooked Teeth
Overlapping or misaligned teeth create hard-to-clean areas where plaque collects. Over time, this buildup can cause gum disease and decay. Using the right toothbrush and focusing on tricky spots can help.
Medical Conditions
Chronic gingivitis can also be linked to other health problems, such as viral or fungal infections. Medications for epilepsy, angina, or high blood pressure may increase the risk as well, so it’s important to let your dentist know about your prescriptions.
How Does Plaque Cause Gingivitis?
Plaque is the main factor behind gingivitis. It’s a soft, sticky layer of bacteria that thrives on leftover food, sugars, and saliva.
- Plaque Formation: Bacteria mix with food debris and saliva.
- Toxin Release: Bacteria release toxins that irritate the gums.
- Inflammation: Gums swell, become tender, and bleed easily.
- Tartar Buildup: Within 48 hours, plaque can harden into tartar, which brushing can’t remove.
The presence of gingivitis plaque on teeth is the earliest visible sign. Regular dental cleanings are essential for controlling tartar buildup.
Do Gingivitis Cuts on Gums Indicate Severity?
Gingivitis itself doesn’t cause cuts, but swollen gums are fragile and prone to injury. Cuts may come from:
- Aggressive brushing with a hard-bristle toothbrush
- Flossing improperly
- Dental appliances (braces, aligners, retainers) rubbing against gums
- Eating hard or sharp foods
These small gingivitis cuts on the gums can worsen inflammation, increase discomfort, and make you more susceptible to infections.
How to Treat Gingivitis?
Treat gum disease depending on how far the condition has developed. In its early stages, gingivitis is reversible and can often be treated with consistent at-home oral care, such as brushing, flossing, and using mouthwash. However, if the disease progresses and plaque hardens into tartar, professional dental treatment becomes necessary. The earlier gingivitis is diagnosed, the easier it is to treat and reverse effectively. Treatment approaches are generally divided into gingivitis home remedies and professional interventions, both of which play an important role in restoring gum health.
At-Home Treatments for Gingivitis

If gingivitis is still mild, you can often reverse it by maintaining proper oral hygiene at home. These simple but effective steps help lay the foundation for healthier gums.
Proper Brushing Technique
Brushing is the first and most important defense against plaque buildup, but the way you brush matters as much as how often you do it. Dentists recommend using a soft-bristle toothbrush to avoid irritating already inflamed gums. Each session should last at least two minutes, twice daily, and should cover every surface of the teeth with special attention to the gumline, where plaque tends to gather. Holding the toothbrush at a 45-degree angle allows the bristles to clean along the gumline more effectively.
Daily Flossing
While brushing is important, it cannot remove the food particles and plaque lodged between teeth. Flossing once a day is critical to preventing the spread of bacteria that cause gum inflammation. When performed correctly, flossing reduces the chances of plaque hardening into tartar, especially in the areas that a toothbrush cannot reach.
Use of Antimicrobial Mouthwash
Incorporating an antimicrobial mouthwash into your daily routine can add an extra layer of protection. Rinses containing ingredients such as chlorhexidine, cetylpyridinium chloride, or natural essential oils like eucalyptus and thymol can help control bacterial growth, soothe inflamed gums, and reduce bad breath caused by gingivitis. While mouthwash should not replace brushing and flossing, it works best as a supportive step in your oral hygiene routine.
Dietary Improvements (H4)
Your diet has a bigger impact on oral health than many realize. Eating a variety of fruits and vegetables, especially foods high in vitamin C, can help strengthen gum tissue and lower inflammation. On the other hand, sugary and acidic foods encourage bacterial growth and plaque buildup. Reducing your intake of processed foods, soda, and sticky candies can lower your risk of gingivitis. Staying well-hydrated also helps, since saliva naturally washes away bacteria and food particles.
Professional Treatments for Gingivitis

If gingivitis has advanced, at-home care alone may not be enough. When tartar buildup and persistent inflammation occur, professional dental treatments are needed. These procedures focus on removing harmful deposits and preventing further damage to the gums.
Dental Cleaning (Scaling and Root Planing)
The most common professional treatment is a dental cleaning performed by a hygienist or dentist. During this procedure, plaque and tartar are removed from above and below the gumline with specialized tools. In more severe cases, a deep-cleaning treatment called scaling and root planing may be necessary. Scaling removes hardened tartar, while root planing smooths the root surfaces of teeth. This helps gums reattach firmly to the teeth and reduces the likelihood of future plaque buildup.
Antibiotic Therapy
If gingivitis has led to significant inflammation or infection, dentists may recommend antibiotic therapy. Options include gels applied directly to the gum pockets, oral antibiotics, or small antiseptic chips placed under the gumline. Antibiotics are generally used in combination with procedures like scaling and root planing to effectively manage infection.
Laser Therapy
Advances in modern dentistry have made laser therapy a highly effective option for treating gum inflammation. Lasers can target and remove inflamed tissue with precision, kill bacteria, and encourage faster healing. This approach is minimally invasive, less painful than traditional methods, and may reduce the need for more aggressive surgery if gingivitis progresses to periodontitis.
Prevention of Gingivitis
Here are the gum disease prevention tips:
Practice Good Oral Care
Preventing gingivitis starts with practicing good oral care every day. Brushing your teeth for at least two minutes, twice a day, once in the morning and again before bed, is essential for removing plaque and bacteria. Flossing at least once daily is equally important, as it clears food particles and plaque from between the teeth where a toothbrush cannot reach. In fact, flossing before brushing helps dislodge debris so it can be brushed away more effectively. For even better results, brushing after every meal or snack, or as your dentist recommends, provides additional protection against plaque buildup.
Go to the Dentist Regularly
Regular dental visits are another critical step in prevention. Seeing your dentist or dental hygienist every 6 to 12 months for professional cleanings helps maintain oral health. Those with risk factors such as dry mouth, smoking, or taking certain medications may need more frequent cleanings to prevent gingivitis from progressing into periodontitis. Annual dental X-rays are also recommended, as they can detect problems not visible during a regular exam and help track changes in your dental health over time.
Take Steps to Lead a Healthy Lifestyle
A healthy lifestyle also plays a big role in protecting your gums. Eating a balanced diet rich in nutrients supports strong gum tissue, while managing conditions such as diabetes can lower the risk of inflammation. Limiting sugar, avoiding tobacco, and maintaining overall health are all important steps to reduce the likelihood of developing gingivitis.
Complications If Gingivitis Is Left Untreated
If gingivitis isn’t treated, it can spread to the gums, teeth, and bones. Possible complications include:
- Gum or jawbone abscesses
- Periodontitis (which may lead to tooth and bone loss)
- Recurrent gingivitis
- Trench mouth (painful, ulcerated gums from infection)
Final Takeaways: Take Gingivitis Seriously
Gingivitis is not just about bleeding gums, it’s an early warning sign of more serious dental problems to come. Spotting the symptoms of gingivitis early, dealing with plaque buildup on the teeth, and preventing gum disease through proper oral hygiene can stop the disease before it progresses.
If you notice any signs of early-stage gingivitis, it’s important not to wait. By improving your oral care routine and seeking professional dental treatment, you can fully reverse the condition. This not only protects your smile but also safeguards your overall health from complications linked to gum disease.
FAQs
1. What is the main cause of gingivitis?
The main cause is plaque buildup on teeth and gums, which harbors bacteria that irritate gum tissue.
2. How do you fix gingivitis?
Gingivitis is reversed with daily brushing, flossing, using mouthwash, and a professional dental cleaning.
3. What does stage 1 gingivitis look like?
Stage 1 shows red, swollen gums that may bleed when brushing or flossing but are not yet painful.
4. Does gingivitis go away on its own?
No. Gingivitis doesn’t go away on its own—it requires good oral hygiene and professional care.
5. Can mouthwash help gingivitis?
Yes. Antibacterial mouthwash helps reduce plaque and bacteria, but works best with brushing and flossing.
6. What happens if gingivitis is untreated?
Untreated gingivitis can progress to periodontitis, leading to gum recession, bone loss, and tooth loss.
7. What can be mistaken for gingivitis?
Conditions such as canker sores, vitamin deficiencies, or allergic reactions can mimic gingivitis symptoms.
8. What is the best toothpaste for gingivitis?
Toothpaste with fluoride and antibacterial agents (like stannous fluoride or triclosan) is recommended.
9. What does periodontitis smell like?
It often causes persistent bad breath (halitosis) due to bacterial infection in the gums.
10. Should I brush my gums with gingivitis?
Yes. Use a soft-bristled toothbrush and gently brush along the gumline to remove plaque without irritation.
11. How to tell if gingivitis is healing?
Healing gums become less red and swollen, bleed less, and feel firmer and healthier.
12. How often should you floss?
Floss at least once daily to remove plaque and food particles between teeth.
Citations:
Gingivitis - Symptoms and causes. (n.d.). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/gingivitis/symptoms-causes/syc-20354453
Institute for Quality and Efficiency in Health Care (IQWiG). (2023, August 23). Overview: Gingivitis and periodontitis. InformedHealth.org - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK279593/
Rathee, M., & Jain, P. (2023, March 27). Gingivitis. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557422/