Table of Contents
- Understanding Herpes on Tongue
- Causes & Triggers of Herpes on Tongue
- Symptoms of Herpes on Tongue
- Diagnosing Herpes on the Tongue: Tests and Clinical Evaluation
- Treatment Options for Herpes on Tongue
- Prevention and Reducing Recurrence of Herpes on Tongue
- Special Considerations & Differential Diagnoses
- Prognosis & Outlook
- Final Thoughts on Herpes on Tongue
- FAQs
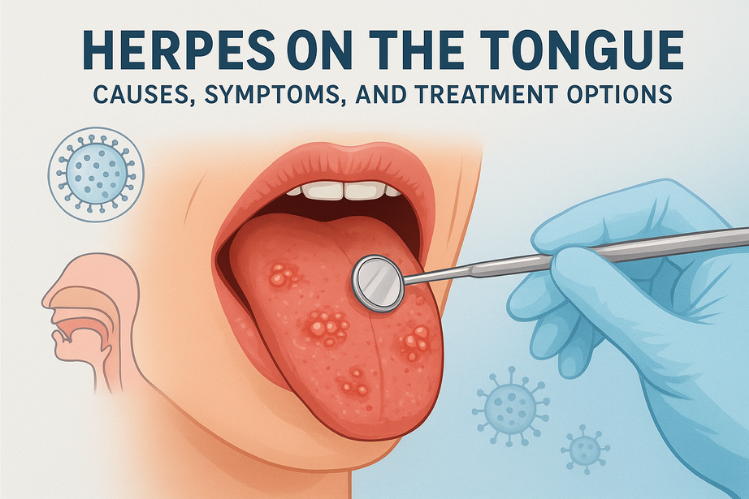
You've probably heard of cold sores, those bothersome blisters that appear on the lips after illness, stress, or too much sun. But what if similar painful bumps show up on your tongue? It's probably not the first idea any of us has had for something herpes related, yet herpes on the tongue is a legitimate condition that is often miscategorized and misunderstood.
Just like any other form of oral herpes, herpes on the tongue can cause symptoms of burning, tingling, and small ulcers that make talking, eating, and swallowing not only inconvenient but sometimes flat-out impossible. Since the tongue is such an integral part of life as we know it, we may feel that an outbreak here would be much worse than a cold sore on the lip.
Understanding what causes herpes on the tongue, how to spot early warning signs, and what treatment modalities actually work can go a long way in comfort and recovery as it relates to herpes on the tongue.
This comprehensive guide provides you with everything you may want to know if it's your first or fifth outbreak, including everything from herpes under tongue, herpes lingual, cold sore on tongue, mouth herpes, herpes on lips, and herpes in mouth.
Understanding Herpes on Tongue
When most people think of herpes, they imagine the typical cold sore on the lips. However, herpes on tongue, though less common, is a form of oral herpes that can cause painful blisters, ulcers, or bumps anywhere on or under the tongue.
The condition is caused by the Herpes Simplex Virus (HSV), a lifelong virus that can reactivate during times of stress, illness, or immune suppression. Once infected, the virus hides within your nerve cells and can reappear in the same or nearby locations during outbreaks.
There are two main strains:
- HSV-1: Typically responsible for oral herpes, including herpes bumps on the tongue, herpes under the tongue, and cold sores around the lips.
- HSV-2: Commonly linked to genital herpes, but can also affect the oral cavity through oral-genital contact.
While not life-threatening, herpes lingual infections can cause significant pain, difficulty eating, and emotional distress, especially during initial outbreaks.
Causes & Triggers of Herpes on Tongue
Now, let’s dive into the causes, risk factors, and other crucial information regarding herpes on tongue.
Causes: How Does It Spread?
Herpes in the oral region, including the tongue, typically spreads in these ways:
- Direct Contact: Kissing or touching someone’s active cold sore, even if the lesions are not yet visible.
- Sharing Items: Lip balm, utensils, straws, toothbrushes, or other objects that come into contact with saliva.
- Autoinoculation: Touching an existing herpes lesion (e.g., on the lip) and then touching another part of your mouth or tongue.
- Oral-genital contact: In cases where HSV-2 is involved, oral-genital contact can lead to oral HSV infection.
Triggers for Reactivation
Even after the initial infection, the virus can reactivate and cause outbreaks on or near the tongue. Some common triggers include:
- Stress, fatigue, or illness
- Sunlight or UV exposure
- Local trauma (e.g., biting tongue, dental work)
- Hormonal changes
- Immunosuppression or other illnesses
Though not everyone experiences frequent reactivation, certain individuals may notice more frequent oral outbreaks.
Symptoms of Herpes on Tongue
Herpes on tongue can present in different ways depending on whether it’s an initial (primary) infection or a recurrent outbreak.
Early / Prodromal Signs (Early Herpes Tongue)
- Before visible lesions appear, you may sense:
- Tingling, itching, burning, or discomfort in a spot on your tongue
- Slight soreness, redness, or irritation
- Mild swelling
These early sensations often precede the formation of visible lesions.
Visible Lesions: Herpes Bumps on Tongue
As the outbreak of oral herpes on tongue progresses, you might see:
- Red, swollen patches or bumps on the tongue (which may later develop fluid-filled blisters)
- Blisters that rupture and lead to shallow ulcers, possibly with yellowish or white crusting or exudate.
- Pain, sensitivity, and burning while eating, drinking, or speaking
- Ulcers or sores may extend to adjacent areas, like the underside (herpes under tongue) or the floor of the mouth.
Because the tongue is a mobile, moist environment, lesions may heal more slowly and cause more discomfort.
Systemic or Associated Symptoms
Especially in a primary outbreak, one may also have:
- Fever, chills
- Malaise, fatigue, body aches
- Swollen lymph nodes (often in the neck)
- Sore throat
- Difficulty swallowing or drooling
- Loss of appetite
These symptoms are more common in an initial infection than in mild recurrences.
When Lesions Overlap with Lips / Mouth
It’s common for herpes affecting the tongue to occur in conjunction with more typical oral herpes, such as a cold sore on the lips or herpes on the lips, or lesions on the gums, cheeks, or the roof of the mouth.
Diagnosing Herpes on the Tongue: Tests and Clinical Evaluation
Recognizing herpes on tongue clinically is based on appearance and symptoms. But to confirm the diagnosis:
- Swab/Culture / PCR: A sample of fluid from a lesion can be tested for HSV DNA or virus.
- Blood Tests (serology): To detect antibodies to HSV-1 or HSV-2 when no lesions are present.
- Clinical Exam: A doctor or dentist will visually examine the lesions and consider the patient’s symptoms and medical history.
It’s important to rule out other oral conditions (e.g., aphthous ulcers, hand-foot-mouth disease, coxsackie virus, traumatic ulcers, fungal infections) that may mimic herpes.
Treatment Options for Herpes on Tongue
Managing herpes on tongue involves a combination of antiviral therapies, pain management, and supportive care. While there is currently no cure for herpes, medical treatment focuses on relieving symptoms, speeding up recovery, reducing viral shedding, and minimizing the chances of future outbreaks.
According to the Cleveland Clinic , once a person contracts the herpes simplex virus (HSV), it remains in the body for life and may reactivate periodically.
General Principles of Treatment
Since herpes is a lifelong viral infection, treatment is primarily aimed at symptom control and outbreak management rather than complete elimination of the virus. Medical experts emphasize that the earlier antiviral treatment begins, ideally within 48 hours of the first symptoms, the more effective it is in reducing the severity and duration of sores. This early intervention helps control the infection before the virus multiplies and spreads to surrounding tissues.
Antiviral Therapies
These are the cornerstones for managing oral herpes outbreaks:
- Oral Antivirals: Acyclovir, valacyclovir, famciclovir. These may be given as episodic therapy (short-term during outbreaks) or suppressive therapy (daily use to reduce recurrence).
- Topical Antivirals/Ointments: Creams such as acyclovir or penciclovir can be used for superficial lesions, though their effectiveness inside the mouth is limited.
- Topical Anesthetics / Numbing Agents: To relieve pain (e.g., lidocaine gel). Use cautiously to avoid over-numbing
Supportive & Self-Care Measures
These measures can ease discomfort and support healing:
- Pain Relief: Over-the-counter NSAIDs (ibuprofen, naproxen) or acetaminophen to reduce pain and inflammation.
- Maintain Hydration: Drink cool, non-acidic fluids. Use a straw if needed to avoid contact with sores.
- Soft, Bland Diet: Avoid spicy, salty, acidic, or rough foods that irritate lesions.
- Oral rinses/Mouthwashes: Gentle antiseptic or saline rinses; medicated rinses (with anesthetic) may help.
- Keep Area Clean & Dry: Avoid additional trauma or irritation.
- Avoid Contact with Lesions: Don’t touch or pick sores. Wash your hands often.
When to Consider Medical or Specialist Care
Seek professional healthcare if:
- This is your first outbreak (to confirm diagnosis and receive guidance)
- The lesions are severe, large, or prolonged
- You cannot eat, drink, or swallow due to pain
- You see multiple lesions or spread beyond the tongue
- You are immunocompromised or have other health conditions
- You experience frequent recurrences and want suppressive therapy
- You notice any unusual signs, like eye involvement, central nervous system symptoms, or worsening systemic signs
In such cases, a doctor may prescribe stronger or intravenous antivirals or refer you to an infectious disease specialist or oral medicine specialist.
Prevention and Reducing Recurrence of Herpes on Tongue
While herpes cannot be eradicated from your body, there are strategies to reduce the risk of acquiring it (if you don’t have it) or to reduce recurrences and transmission if you do.
Preventing Spread (If You Have Oral HSV)
- Avoid kissing, sharing utensils, cups, lip products, or oral contact during active outbreaks
- Use barrier protection (like dental dams) during oral-genital contact
- Wash your hands thoroughly, especially after touching your mouth or lesions
- Don’t touch one lesion and then other areas of your mouth
- Be cautious of asymptomatic viral shedding (you may transmit even without visible lesions).
Reducing Triggers & Frequency of Outbreaks
- Manage stress and get adequate rest
- Use lip balm with sunscreen to reduce sun-induced reactivation
- Avoid trauma to the lips or mouth
- Keep the immune system healthy (nutritious diet, good sleep, exercise)
- Some people with frequent outbreaks may benefit from daily suppressive antiviral therapy as prescribed by a doctor
Special Considerations & Differential Diagnoses

It’s essential to distinguish herpes on the tongue from other oral conditions. Sometimes, it’s just canker sores or other infections or lesions. And they can present similar symptoms.
So, here’s what to look out for:
Distinguishing from Canker Sores or Aphthous Ulcers
Canker sores are non-herpetic and usually non-contagious. They appear inside the mouth (including under the tongue) and often present as round or oval ulcerations with a white or yellow center and red border. They typically don’t follow a tingling prodrome and aren’t caused by HSV.
Herpetic Stomatitis / Gingivostomatitis
In children or during a primary infection, herpes may present as herpetic stomatitis, affecting multiple areas of the oral cavity (tongue, gums, inner cheeks). This often involves fever, pain, drooling, and multiple lesions.
Other Infections & Conditions
- Viral infections (e.g., Coxsackie virus, hand-foot-mouth disease)
- Fungal (e.g., thrush)
- Traumatic ulcers (biting, burns)
- Allergic reactions, lichen planus, or oral cancer (rare)
If lesions persist for long (weeks) or don’t respond to treatment, further evaluation is warranted.
Prognosis & Outlook
- Most herpes lesions heal within 1–3 weeks with supportive care; prompt antiviral therapy can reduce healing time.
- Over time, many people experience fewer outbreaks as the immune system adapts.
- Recurrences tend to be milder than the first episode
- Good management, avoiding triggers, and, when needed, suppressive therapy can significantly reduce discomfort and frequency
Final Thoughts on Herpes on Tongue
Herpes on tongue is a less common, but possible, manifestation of oral herpes (HSV-1 or less commonly HSV-2). It may present with tingling and early discomfort, followed by herpes bumps on the tongue, blisters, ulcers, and pain, especially when eating or speaking. Diagnosis is often clinical but can be confirmed via swab or lab testing.
While there is no cure, antiviral medications (oral and topical in some cases) are effective in reducing the severity and duration of outbreaks, especially when started early. Supportive care, pain relief, hydration, soft diet are essential. Preventive measures and careful oral hygiene help reduce transmission and recurrence.
If you think you might have herpes on your tongue, especially if it’s your first such episode or if symptoms are severe or prolonged, it’s best to consult a qualified medical or dental professional for evaluation and guidance.
FAQs
1. How do you treat herpes on tongue?
Treatment includes antiviral medications like acyclovir or valacyclovir, topical pain relievers, and maintaining good oral hygiene to reduce discomfort and speed healing.
2. What can be mistaken for herpes on tongue?
Conditions like canker sores, allergic reactions, oral thrush, or geographic tongue can resemble herpes blisters.
3. How do I know if I have oral herpes in my mouth?
You may notice painful blisters or ulcers on the tongue, lips, or inside the mouth, often accompanied by burning or tingling sensations.
4. How can I boost my immune system to fight herpes?
Eat a balanced diet, manage stress, get enough sleep, stay hydrated, and avoid smoking or excessive alcohol to strengthen immunity.
5. What are common herpes triggers?
Common triggers for oral herpes outbreaks include stress, illness, sun exposure, hormonal changes, fatigue, and weakened immunity. Dental work or trauma to the mouth may also activate the virus. Identifying and managing your personal triggers is key to preventing frequent recurrences.
6. Does oral herpes go away?
While oral herpes cannot be cured, the sores typically heal within 7 to 14 days. The virus remains dormant in nerve cells and may reactivate during periods of stress or weakened immunity. Antiviral treatments and preventive care help shorten healing time and reduce recurrence.
7. What is the best treatment for oral herpes?
Prescription antivirals like acyclovir, valacyclovir, or famciclovir are the most effective treatments for reducing outbreak duration and severity.
Citations:
Whitley, R. J., & Roizman, B. (2001). Herpes simplex virus infections. Lancet, 357(9267), 1513–1518. https://doi.org/10.1016/S0140-6736(00)04638-9
Arshad, Z., Alturkistani, A., Brindley, D., Lam, C., Foley, K., & Meinert, E. (2019). Tools for the diagnosis of Herpes Simplex Virus 1/2: Systematic review of studies published between 2012 and 2018. JMIR Public Health and Surveillance, 5(2), e14216. https://doi.org/10.2196/14216